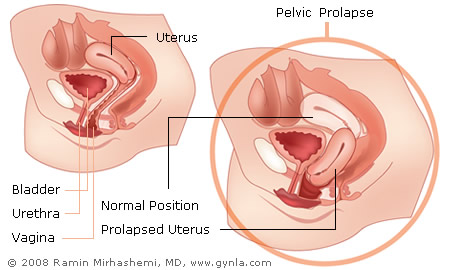
Pelvic prolapse in women is a very common condition that is sometimes avoided by patients and their caretakers. This is a general term that describes the weakening of the tissues, and ligaments that give support to the uterus, vagina, bladder, and rectum. Some of the risk factors for pelvic prolapse include, multiple vaginal births, especially large babies, prolonged labor, chronic conditions such as diabetes, COPD (chronic obstructive pulmonary disease), obesity, and finally genetic factors.
Many women do not have symptoms with pelvic organ prolapse. However, some may notice a bulge or lump in the vagina or notice the vagina protruding outside the body. Other pelvic prolapse symptoms may include:
- A pulling or stretching feeling in the groin area
- Delayed or slow urinary stream
- Difficulty with bowel movements
- Painful sexual intercourse
- Urinary and fecal incontinence
- Vaginal pain, pressure, irritation, bleeding or spotting
Dr. Mirhashemi is trained in the field of urogynecology and pelvic reconstructive surgery.

Non-surgical pelvic prolapse treatment can be 60 to 70% successful if the prolapse is identified early. These non-invasive pelvic prolapse repair modalities include Kegel exercises, biofeedback, and the use of pessaries. If pelvic reconstructive surgery is required, you can be assured that Dr. Mirhashemi will provide the best and most up-to-date pelvic prolapse treatment options for your particular case. Dr. Mirhashemi is trained in the field of urogynecology and pelvic reconstructive surgery.
Pelvic reconstructive surgery should accomplish two specific goals:
- To restore the organ that has shifted to its natural position and reinforce it in place
- To reinforce the pelvic floor muscles in the weakened area so that further damage will not occur
This can be accomplished using many different surgical pelvic prolapse treatments. Often organs are fixed and anchored to the ligaments where they were torn from, such as tissues around the pubic bone. In certain cases, where the tissues are friable and weak, a mesh (a synthetic material sometimes referred to as a hammock) may be used. Over time, the body grows stronger tissue into this synthetic material and gives it further support. Before having pelvic reconstructive surgery, Dr. Mirhashemi will ensure that the diagnosis is accurate so that you receive the appropriate surgery. This may include performing cystoscopy, urodynamic studies, or a defecogram.
Please refer to the following links for more information:
• American Urogynecologic Society (AUGS) Cystocele (Fallen Bladder) (National Kidney and Urologic Diseases Information Clearinghouse)
• How to Use a Pessary (American Academy of Family Physicians)