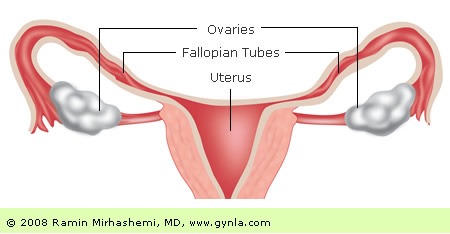
Ovarian cancer is one of the most common types of cancers in women. It occurs when cells in the ovaries begin to abnormally multiply and eventually form a tumor. Ovarian cancer affects about 22,000 women every year, and it can be very difficult to detect in its early stages.
Cancerous tumors in the ovaries can grow over time and spread to other parts of the body. This is one of the reasons why early detection and effective treatment is important. At GYN LA, we offer advanced cancer treatment options that help women deal with this condition. We are experts at hernia treatment, hysterectomy, Pelvic Prolapse Surgery, uterine fibroids, and much more.
There are 3 main types of cells in the ovaries, all of which can cause a different type of ovarian cancer. The most common type of cells (in the ovaries) are epithelial cells. These cells line the outer surface of the ovary and are the most likely to develop epithelial cell tumors. The cells that produce eggs (germ cells) can also develop germ cell tumors. And finally, stromal tumors arise from the structural cell tissues that hold the ovary together.
Symptoms of Ovarian Cancer
Ovarian cancer can be very difficult to detect. This is because most cancers are only detected once they get to an advanced stage and begin exhibiting symptoms. In fact, ovarian cancer is commonly detected once the tumor is large enough to affect the functions of bodily organs- or cause pain/bleeding in various parts of the body.
Ovarian cancer typically begins in the ovaries and spreads to other organs in the abdomen. During this spreading phase, patients don’t feel any type of pain. Pain only sets in when the tumor is large enough to affect the abdomen and other nearby organs.
Some of the symptoms of ovarian cancer include:
- The feeling of a constantly bloated stomach
- Pain and discomfort in the tummy area
- A feeling of peeing
- Frequent fatigue
- Heartburn and constipation
- Back pain
- Pain during intercourse
- Irregular menstruation
The challenge with ovarian cancer symptoms is that they resemble many different health complications. Most patients don’t realize that they have ovarian cancer, confusing their condition for other diseases and ailments. While ovarian cancer-like symptoms may point to a different condition, they tend to persist if they’re actually associated with ovarian cancer.
Possible Causes
Currently, there is no clearly established cause of ovarian cancer. However, research has identified various risk factors that expose women to contracting this condition. In general, cancer is caused by mutations in DNA. These mutations result in the growth of abnormal tissues that eventually create tumors. When these tumors metastasize (spread to other parts of the body), the cancerous condition can significantly worsen.
The following are possible causes and risk factors associated with ovarian cancer.
- Old age
Ovarian cancer most commonly occurs in women aged 50-60 years.
- Gene mutations
Certain gene types can increase your risk of ovarian cancer. These genes- BRCA1 (Breast Cancer Gene 1) and BRCA2 are also the genes responsible for increasing one’s risk of breast cancer.
- The age of a woman’s menstrual cycle
The risk of ovarian cancer is also increased when women start their menstrual cycle early or reach menopause late.
- Family history
A family history of ovarian cancer also increases one’s risk of contracting the disease. In addition, if you’ve had breast cancer, colon, or uterine cancer, your risk of contracting ovarian cancer is also higher.
- Obesity
Weight and obesity can have an impact as a possible cause.
- Hormone replacement therapy
Patients who’ve undergone hormone replacement therapies (such as estrogen replacement) or have used fertility drugs may also be at higher risk of contracting ovarian cancer.
How Ovarian Cancer Be Diagnosed
Diagnosing ovarian cancer at an early stage is key to treating this condition. However, this is easier said than done. The ovaries are deeply embedded in the abdominal cavity, and small tumors are not easy to detect.
Most diagnoses are done via a pelvic exam where doctors can detect irregularities in the ovaries. In addition, larger tumors are easier to detect because they exert pressure on the bladder and rectum.
At GYN LA, our experienced physicians can detect ovarian cancer in its early stages. We use advanced screening tests that meet the following criteria.
- Testing for pre-cancerous changes
Our testing process begins with techniques that can detect your risk factors to contracting ovarian cancer. Our goal is to prevent people from getting cancer, and hence we use a combination of techniques that can detect any changes in the cervical area. These changes typically point to the possible development of cancer.
- An affordable testing process for our patients
We also design our testing process to be affordable to patients. This inexpensive process encourages women to come in for regular testing and early detection of ovarian cancer risk factors.
- A painless test
Many women associate cancer screening with pain and discomfort. This is often enough reason to keep women away from carrying out yearly mammography. Our testing process is painless and less intrusive, allowing women to come in for regular testing.
- Effective identification of abnormal test results
In most cases, smaller organs such as the breast and cervix are easier to positively biopsy for cancer. Other larger organs (such as the ovaries) may be more complicated to gain conclusively positive results. During our testing process, we try to ensure that the organ being biopsied yields accurate results (whether positive or negative).
Ovarian Cancer Treatment
At GYN LA, we specialize in many different oncological procedures. We diagnose and treat many various types of cancer, from cervical to vaginal and ovarian cancer. We also use robotic surgery procedures to carry out myomectomy, hysterectomy, and sacrocolpopexy.
In our treatment of ovarian cancer, our patient-centered care for women covers comprehensive services that instill confidence, comfort, and compassion. Here are some of our oncology related services you can expect to receive from GYN LA.
- GYN Expertise
- Hernia Treatment
Hernia typically refers to a weakened abdominal wall that occurs after undergoing abdominal surgery. A weakened wall can result in little support to your pelvic organs.
At GYN LA, we can implant a sterile surgical mesh that will strengthen your abdominal wall. This mesh is also compatible with internal body tissues and abdominal cells can easily grow around it to result in a much stronger vaginal wall.
- Hysterectomy
A Hysterectomy involves surgical removal of the uterus due to a gynecologic malignancy, a pre-cancerous condition, or a benign pelvic problem. We carry out different types of Hysterectomies, with each type being defined by how the removal is carried out.
Our Hysterectomies involve robotic-assisted approaches, trans-abdominal, trans-vaginal, and laparoscopic approaches.
-
Laparoscopic Surgery
Minimally invasive surgeries are becoming a preferred option for many patients in the country and around the world. Laparoscopic surgery is a minimally invasive technique used to treat laparoscopic benign and malignant gynecologic conditions. At GYN LA, our own Dr. Mirhashemi carries out Laparoscopic surgery to help patients recover faster and achieve better aesthetic results.
-
Management of Abnormal Pap Smears
Every year, many women worry about having abnormal Pap smear results. However, abnormal results are quite “normal” and they may indicate many different things.
We carry out new FDA-approved Pap smear tests that are more targeted and effective at indicating many different conditions. The Thinprep and Autocyte Pap smears that we carry out are more sensitive and specific in nature.
-
Pelvic Prolapse Surgery
A pelvic prolapse is a condition where tissues that support your uterus, vagina, bladder, and rectum become weakened. A pelvic prolapse often occurs in women who have had multiple vaginal births, prolonged periods of labor, and conditions such as diabetes. Having weakened abdominal walls often results in symptoms such as slow urination, painful sex, complications with bowel movement, vaginal pain, and irritation.
At GYN LA, our pelvic prolapse surgery involves restoration of the organ to its natural position and reinforcing the pelvic floor muscles in the weakened area against further damage.
-
Urinary Incontinence
Urinary incontinence is the condition where one is unable to control the passing of urine from their bladder. This condition affects millions of women and can cause intense emotional distress.
At GYN LA, we treat all 3 types of urinary incontinence, including stress and urgent incontinence. We understand how stressful this condition can be. That is why our treatment options consider both the medical and psychological components that this condition has on millions of women.
-
Vulvar Disease
Vulvar disease is a condition that affects women’s external genitalia. It can manifest itself in many different ways, from infectious to inflammatory and pre-cancerous conditions. Vulvar disease may also occur as a vulvar dystrophy (change in the skin around the vulva) or as a pre-cancerous change.
We offer accurate diagnostic testing and therapy to restore normal function in these affected areas.
-
Uterine Fibroids
Affecting 33% of women in the U.S, uterine fibroids refer to non-cancerous growths that occur along the inner muscular wall of the uterus. The symptoms of uterine fibroids include irregular bleeding, lower back pain, heavy menstrual cycles, and bladder symptoms.
We can diagnose uterine fibroids using an ultrasound, MRI, CT scan, or hysteroscopy. We can then treat the condition in multiple ways, including a hysterectomy, myomectomy, or uterine artery embolization.
- Hernia Treatment
- da Vinci Robotic Surgery
GYN LA provides robotic surgical procedures that are designed to deliver the best possible care. We have taken the initiative to provide innovative and comprehensive treatment options for women of all ages.
Our da Vinci Robotic Surgery involves the following:
- Robotic Sacrocolpopexy
Robotic Sacrocolpopexy is a surgical procedure that is used to fix pelvic organ prolapse. It can be used to address prolapse in the uterus, vagina, or cervix.
During Sobotic Sacrocolpopexy, a laparoscope is used to view the surgical site and fix prolapse issues without needing to make a large incision. This procedure results in relief of uncomfortable pressure in the vagina, relief of uncontrollable urges to urinate, and relief of vaginal pain (among others).
-
Robotic Myomectomy
The da Vinci Robotic Myomectomy is a procedure useful in removing fibroids. This technique can address fibroid complications without affecting the uterus lining. During this procedure, a precise incision can be made to remove the fibroid by using a highly accurate camera.
Because the surgeon will have a clear vision of the surgical site, patients will enjoy more accurate results and quicker recovery times.
-
Robotic Hysterectomy
A robotic hysterectomy refers to the surgical removal of a woman’s uterus. Through a combination of advanced imaging techniques and the da Vinci Surgical System, the specialists at GYN LA can safely and efficiently carry out a hysterectomy using minimally invasive techniques. A robotic hysterectomy results in shorter recovery times, less blood loss, and minimal scarring to the incision site.
- Robotic Sacrocolpopexy
- Gynecology Oncology
GYN LA also specializes in diagnosing and treating various forms of cancer. We use advanced diagnostic and treatment procedures that increase the chances of our patients making a full recovery. Among the types of cancer we diagnose and treat include:
- Cervical Cancer:
Cancer of the cervix is often caused by heavy smoking, untreated HPV, and a lack of Pap smear tests. It can result in abnormal bleeding of the vagina, pelvic pain, irregular bleeding, among other symptoms.
-
Endometrial/Uterine Cancer:
As the most common gynecologic cancer in the country, uterine cancer arises from abnormal cells in the inner uterus lining. There are two main types: type 1 and type 2, and each can cause painful urination, pelvic pain, bleeding of the uterus, among other symptoms. We can diagnose uterine cancer through an endometrial biopsy or a dilatation and curettage.
-
Menopause/Hormonal Replacement Therapy:
Hormone replacement therapy (HRT) can help women who have recently hit menopause to restore their natural hormonal balance. HRT helps many older women to lead normal lives and to minimize the undesirable effects of menopause.
-
Vaginal Cancer:
Vaginal cancer can occur as either a squamous cell carcinoma (cancer affecting the lining of the vaginal surface) or as an Adenocarcinoma (cancer affecting the glandular cells). Vaginal cancer can cause pain in the pelvis, pain during intercourse, and a lump in the vagina.
-
Vulvar Cancer:
Vulva cancer primarily affects the inner and outer lips of the vagina. A tumor typically begins slow growth and develops into a larger structure over time. It is symbolized by a lump in the vulva, itching, tenderness, and bleeding near the vulva region.
-
Uterine Sarcoma:
A uterine sarcoma typically occurs on the muscle layer of the uterus. They can cause bleeding, lumps, frequent urination, and pain in the abdomen. Treatment is typically administered via surgery, radiation and chemotherapy, and hormone therapy.
- Cervical Cancer:
Why is ovarian cancer so hard to detect?
Actually, most cancers are difficult to detect. Most of the time a cancer is not found until it produces some type of symptom and is already fairly advanced.
This usually requires that the cancer
- Be fairly large so that it affects the function of an organ (e.g. ovarian cancer),
- Erode into a mucosal surface and cause bleeding (e.g. colon cancer), or
- Cause pain (e.g. bone metastases).
Ovarian cancer does not erode into organs and, therefore, does not cause any unusual bleeding from the colon or vagina. As it progresses ovarian cancer spreads along the surface of organs in the abdomen and does not produce any type of pain. It is only when the volume of the cancer is great enough to cause some abdominal distension that it makes itself obvious. Since the female pelvis is designed to accommodate large objects (e.g. pregnant uterus) the total amount of tumor present before any symptoms are produced can be in the kilogram range.
You may have read that the symptoms of ovarian cancer include abdominal bloating, constipation/diarrhea, and “gassiness”. However, if I was to take a poll of a random sample of men or women over age 50 how many would admit to these same symptoms on occasion? My guess is that most people would do so. There really is no specific early symptom of this cancer (or most cancers).
Contacting an Ovarian Cancer Specialist Near Me
Women of all ages, and facing many different gynecological conditions, can be seen, diagnosed, and treated by the professionals at GYN LA. Our unique blend of expertise and patient-centered care will put you on the path towards addressing your gynecological health complications and finding solutions that work best for you. We focus on each patient and their individual health needs in order to create a treatment plan that is comfortable and effective.
Need surgery, diagnosis, or just a consultation to learn more about your gynecologic health? Contact GYN LA today at 310-375-8446.
Question and Answers
Yes and no.
A screening test for any cancer should ideally meet several criteria:
- The test should detect a pre-cancerous change. This would allow treatment before a cancer appears. After all, we want to prevent people from ever getting a cancer! Pap smears, for instance, are meant to detect changes in the cervix that precede the development of a cancer (the Pap smear is not very reliable once a cancer is already present).
- The test should be inexpensive. One reason that yearly colonoscopies are not recommended for colo-rectal cancer screening is the cost of the procedure. Pap smears are probably the best example of a screening tool that is relatively inexpensive.
- The test should be painless. This may seem obvious but it is one reason why many women do not get yearly mammography.
- An abnormal test should be easily confirmed. Histologic confirmation of an abnormal screening test requires biopsy of the suspect organ. Some areas of the body are relatively easy to biopsy (e.g. breast, cervix, colon). Other areas of the body are not so easy to biopsy (e.g. brain, bone) and preclude any type of confirmatory test. We always hope that the results of a biopsy accurately predict what is happening in the organ being biopsied but this is not always the case. Biopsy of a small object such as a 5mm breast mass is more likely to accurately rule in/out a the presence of an early cancer than is biopsy of a larger structure such as a 4cm ovary.
- The test should have both a high positive and negative predictive value. Since no test is 100% sensitive and specific the predictive power of any test is far less than perfect. This downside is overcome by only using the test in a population of patients where the prevalence of the pre-malignant condition or cancer being studied is moderately high. Let’s consider 2 examples, pre-malignant changes of the cervix and cancer of the ovary. At any given time 1 in 20 (5%) sexually active women will have a pre-malignant abnormality of the cervix. A pap smear performed on these 20 women will detect the 1 woman with a real abnormality and will falsely predict that an additional 2 women have pre-malignant abnormality (90% specificity).
At any given time 1 in 2500 women will have an ovarian cancer. A screening test with the same specificity as a pap smear would falsely predict that 250 of these women have an ovarian cancer! Even if a screening test was 99% specific it would falsely predict a cancer in 25 women! A screening test for ovarian cancer, like most cancers, is not a real possibility for the following reasons:
- No pre-malignant change in the ovary has been identified (this is the case for most cancers).
- Confirmation of a screening abnormality would require histologic confirmation. The only way to prove that an ovary is not harboring an early cancer is to remove the entire ovary for histologic evaluation. This would require surgical removal of both ovaries.
- To date no population with a moderately high risk of ovarian cancer has been identified. Interestingly, a familial type of ovarian cancer genetic risk has been identified in some families. This familial tendency induces an extremely high lifetime risk of developing an ovarian malignancy. Women in these families are encouraged to have prophylactic removal of the ovaries once childbearing is completed.
It’s not all bad news, however. We actually can determine familial risk with a blood test that can detect mutations in a gene, BRCA1 that, if present, redisposes to the development of both breast and ovarian cancer. This test is very expensive (e.g. $2000) and is only covered by most insurance plans and Medicare if an evaluation by a Genetic Counselor determines the likelihood of a familial tendency. We will talk to you about this test if other members of your family had had either of these cancers.
It all depends on how you look at it.
It is true that the majority of ovarian cancers are not diagnosed until fairly advanced. However, as noted above, the same can be said for most cancers!
It helps to put things in perspective. Of all the cancers that arise in the abdominal cavity (e.g. colon, stomach, liver, uterus, etc) ovarian cancer has the highest cure rate stage-for-stage!
As an example, consider stage 1 cancers of the ovary (the cancer has not yet spread beyond the ovary). Only 5% of ovarian cancers will be found when still stage 1 but these women can expect a 90% likelihood of cure! This is higher than the cure rate of any other abdominal cancer found in Stage 1.
As another example, consider stage 3 cancers of the ovary (the cancer has grossly spread into the upper abdomen). The majority of ovarian cancer patients will present with stage 3 disease. These women can expect a 50% likelihood of cure. On the other hand, a patient with any other type of abdominal cancer presenting with disease this extensive can expect a 0% likelihood of
cure!
Like most cancers there can be no “margin of error” in the proper treatment of an ovarian malignancy if these high cure rates are to be attained. Everything has to be done in the right way at the right time in order to optimize cure rates. This means that the treatment of an ovarian cancer will almost always require an initial surgical procedure with a very simple goal……removal of all visible tumor. Sometimes this is relatively easy to do and sometimes it is much more difficult. Surgery is followed by chemotherapy for 12 to 14 months. It’s not easy but the outcome is worth it!
Wouldn’t it be nice to have a magical test that could detect the presence of one cancer cell? Well, until we have such a test we have to rely on a battery of less-than-perfect tests.
You will be seen for a follow-up visit at 3 month intervals after completion of chemotherapy until you hit the 2-year anniversary of your diagnosis. After that point you will be seen at 6 month intervals until the 5-year anniversary. At each visit you will be given a pelvic exam to detect any “nodularity” in the bottom part of the pelvis (cul-de-sac). This is a sensitive indicator of recurrent tumor in the pelvis. You will also have a CA125 determination at each visit. At regular intervals, usually about every 6 months, you will get a series of CT scans (chest, abdomen and pelvis). This is continued until the 2-year anniversary of your diagnosis. After this point the likelihood of a recurrence is small enough to stop routine surveillance CT scanning.
After 5 years of follow-up we pass the baton to your Primary Physician (after all, you don’t want to have to see an Oncologist any longer than you absolutely have to!).